7. Back Pain
Posted by Phil Heler on December 6, 2015Though less common in athletes, spinal pain can still affect runners, cyclists, golfers and tennis players. Pain can be felt in the facet joints, the ribs, or from trapped nerves caused by disc problems.
Spinal pain – facet joints
Typical symptoms for facet joint pain: Local sharp spinal pain with muscle guarding that can refer into the mid-back, lower back and groin, hip and sometimes upper thigh. This pain usually appears with specific movements (such as twisting and leaning back).
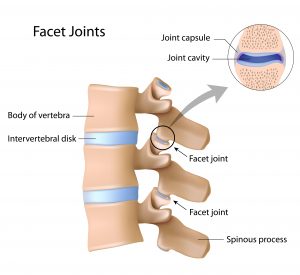
In the spine, facet joints link the vertebrae and are important for preventing excessive rotational and twisting forces which would damage the discs. They also share some of the load bearing of the spine.
When there is a loss of mobility in the spine, the facet joints bear a greater load than normal. This is particularly the case if there is some imbalance in the body and one side of the spine takes more strain than the other. This can occur for all sorts of reasons such as repetitive strain injury through repeated lifting or one single lift in an awkward position or through sudden trauma such as falling on ice. Common day-to-day examples are digging in the garden, hoovering at home or repeated manual handling events in the workplace. It is important to remember that putting the spine under sustained constant load over time is also detrimental. An example would be driving over long distances or the cumulative effects of sitting for long periods during long-haul flights.
People usually experience sharp pain for particular movements such as leaning back or twisting or bending forwards. Pain can be unilateral or bilateral and can sometimes refer into the upper buttock region.
Spinal pain – rib joint pain
Typical symptoms for rib joint pain: Pain between the shoulder blades that is a burning, sharp or stabbing and is capable of referring to the front of your chest. Taking a deep breath or coughing/sneezing can make your rib pain worse.
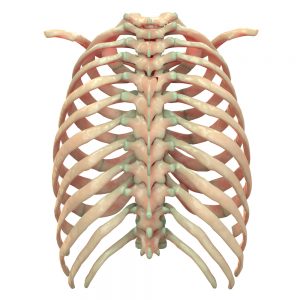
Your rib cage is made up of twelve pairs of ribs. All twelve ribs attach to the middle of your back (or thoracic spine), but only the top seven ribs form your rib cage and attach to the breastbone on the front of your chest. The ribs essentially act as a mean of protecting and guarding all your vital internal organs. Their other function is to lift and drop as part of inhalation and exhalation, which is why rib pain often results in pain when breathing deeply or coughing or sneezing. The lower ribs can be a cause of mid and lower back back pain and similarly the upper ribs can refer pain in the upper thoracic regions.
For each rib there are two joints that attach to any specific vertebra in the thoracic spine. These joints are called the costotransverse or costovertebral joints. The ribs are also anchored by the bodies of the vertebra to which they attach and the intervertebral discs.
These joints can be a common cause of pain. Common causes are a singular traumatic event like a sudden impact in contact sports or as part of a symptom pattern resulting from repetitive strain injury. It is also worth mentioning that very occasionally we can have an extra rib at the top of the spine (called a cervical rib) that can irritate delicate nerves and vascular structures in the surrounding tissue.
Spinal pain – muscular pain in the mid-back
Typical symptoms in the mid-back: Pain on the inside of the shoulder blades that increases with shoulder movements.
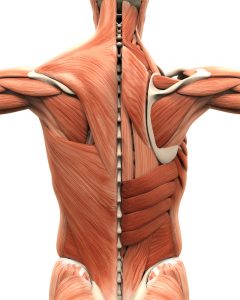
The most common cause of thoracic mid-back pain comes from muscular irritation or other associated soft tissue problems. These can arise from overuse injuries that are common in any sport that is unilateral (i.e. from one side), such as racket sports. Trauma, a frequent component seen in contact sports, or lifting or throwing based sports are other common issues.
The shoulder blade is integral to shoulder movement involving throwing or lifting. Many of the muscles associated with these movements (such as Rhomboids, Trapezius, Latissmus dorsi) can cause back pain. Many of the other muscles responsible for rotation/movement in the neck can also refer pain to the upper back as well. Soft tissue symptoms can also be involved with rib pain or spinal joint pain (refer spinal joint pain) or whiplash injuries.
Spinal pain – muscular pain in the lower back
Typical symptoms in the lower back: Pain that is exacerbated by any movement that stretches the affected muscle or muscle group.
Soft tissue structures in the spine control movement of the spine. They are also the main tissues surrounding the spinal chord and as such will be involved in traumatic or repetitive injuries.
This often evolves from repeated movements such as serving in tennis or a golf swing. Issues that generate constant loading such as cycling or rowing will also affect the lower back anatomy.
There are briefly three groups of muscles in the lower back:
- There are a lot of tiny muscles that help connect the vertebra together (intertransverse and interspinales muscles) that are not responsible for executing movement but do have a big role in proprioreception (sense of joint position). Some of these muscles, however, such as multifidus, do also actually help control the vertebra when bending backwards or forwards.
- Main muscles in front and the side of the lower back are the psoas muscle and quadratus lumborum. The psoas muscle (joins the lower back to the hip) can cause compression on the lower back when you flex your hip. The quadratus lumborum has an action in side-bending the spine.
- Erector spinae. These muscles help anchor the lower back to the pelvis are also commonly involved.
Trapped nerves from herniated or bulging discs
Our new IDD Therapy programme can help treat trapped nerves caused by spinal injuries, is non-invasive (unlike surgery) and is pain-free. IDD Therapy bridges the gap between what manual therapy cannot achieve and surgery. This therapy is the fastest-growing therapy for trapped nerves and degenerative disc issues in the UK.
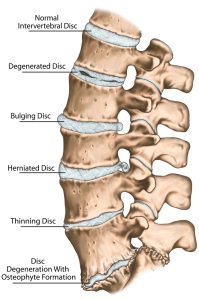
There are a few terms commonly used when describing discs which we can quickly clarify:
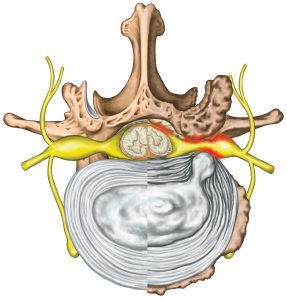
A disc bulge is where the outer wall of the disc bulges out from its normal position. The disc wall is not broken and the nucleus material is contained inside the disc. As the disc bulges, it may press against nerves directly, or the bulge is associated with a loss of disc height and this may lead to impingement of a nerve as it exits the spinal canal though the gap between two vertebrae.
A herniated disc is the same as a prolapsed disc. This is where the nucleus of the disc breaks through the outer disc wall. There will be a loss of disc height as the disc loses pressure and the nucleus material can press directly on to the spinal nerves causing pain. Or the material of the disc nucleus may act as a biochemical irritation to the nerve in which case the result is the same… back pain!
A ‘slipped disc’ is an everyday expression which doesn’t have a true medical definition. It can imply a disc bulge or a herniation, usually a herniation.
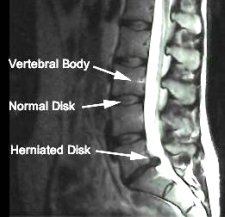
The MRI below demonstrates a herniated disc pressing on nerves. The nerves are demonstrated by the broad white descending line seen in the scan. This is the spinal chord and departing spinal nerves. If you look carefully you can see the herniation making contact with these delicate structures.
The resulting pain from a herniated disc will often refer (hence the term radicular pain) down the pathway of a nerve and into the limb it innervates ,causing either sciatica (in the case of the lower back) or pain into the neck, shoulder and arm (if in the neck). This can often be accompanied with pins and needles in the foot or hand depending on this location.
Our new IDD Therapy programme can help treat trapped nerves, is non-invasive (unlike surgery) and is pain-free. IDD Therapy bridges the gap between what manual therapy cannot achieve and surgery. This therapy is the fastest-growing therapy for trapped nerves and degenerative disc issues in the UK.