Migraine Physiology
Posted by Phil Heler, MD on December 13, 2019There's very little written about migraine physiology, or what a migraine looks like.

Migraine physiology, or what a migraine looks like, is a topic that not much is written about.
Last week’s blog addressed the chemistry of stress and how we can potentially become hardwired into a fight or flight response. One of the key issues with a chronic long-term exposure to stress is the evolution of physical pain. This comes in several forms.
How Migraines and Stress are Closely Connected
Stress is unfortunately often a trigger for events such as headaches and migraines. Migraines affect around 1 in every 5 women and around 1 in every 15 men. They usually begin in early adulthood and can be as frequent as several times a week, although others only have them occasionally. It is possible for years to pass between them.
Migraine and stress are inextricably linked in migraine physiology. Stress as a trigger for migraine attacks is present in nearly 70% of individuals. To make matters worse migraines often result in a negative feedback loop. Stress causes migraine, chronic pain creates more stress—and so the cycle continues. And, to add insult to injury, when, after a busy and stressful week at work, migraine sufferers can also experience a migraine at the weekend as they unwind. If your body is accustomed to constant stress, a weekend off can result in what is termed a “let down” migraine when your stress abruptly lowers. Not exactly a win-win situation either!
Although the causes of migraine are not yet fully understood, both your environment and your genetics each share a roll. In fact, if one or both of your parents has migraines, you are also more likely to experience migraines yourself. A child with one parent who suffers from migraines has about a 50% chance of developing a migraine. If both parents have migraines, the child’s risk is 75%. Recently, a new gene-sequencing technology called Genome-Wide Association Study (GWAS) has helped researchers begin to identify specific genes that may lead to development of migraines. This technique compares DNA from individuals with migraines to similar individuals without migraines. One GWAS analysis looked at the DNA of more than 23,000 migraine sufferers and compared it with DNA from more than 95,000 individuals without migraines. This analysis found 12 specific areas of DNA that appeared to be associated with migraines. It is however important to remember that DNA differences do not actually cause migraines — rather, they make your body function differently, thus possibly heightening the likelihood that migraine triggers will affect you.
Migraine Physiology: What Happens When A Migraine Strikes
The global prevalence of migraine as a primary headache has been estimated as 14.4% in both men and women. One key fact which does surprise me is that migraine headaches have been ranked as the highest contributor to disability in the under 50 year old population in the world. Subsequently a lot of research has been conducted in order to clarify the exact mechanisms of migraine physiology. Although there are still obvious uncertainties, most of the research appears to agree on several key causative possibilities that lead to migraine generation.
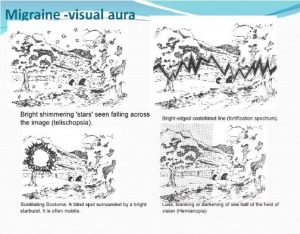
Research appears to be gradually converging in agreement on the concept of cortical spreading depression (or CSD); a proper jargon term! This phenomenon is probably responsible for the aura that many migraine sufferers experience. Migraine with aura occurs in 30–40% of patients who most commonly present with a visual disturbance such as those as in the pictures below.
The visual disturbances can be quite complex including all sorts of really intimidating terms that include ‘fortification spectra’ and ‘photopsia’ or ‘teleschopsia’ and the bizarre term ‘scintillating scotoma’. Fortification spectra are complicated images that can float in your vision during a migraine. These get their name apparently from their resemblance to an aerial view of an intricately built fortified town as seen below!
Photopsia is the word for a complex array of lights and images that appear before your eyes. The most common aura is however a scintillating scotoma. These are shimmering or coloured lines that enlarge over 10 – 20 minutes. While visual symptoms are the most commonly described aura events of migraine there are other symptoms as well. Sensory symptoms including abnormal sensations such as pins and needles which occur over various limbs, occurring in 36% of people, 10% of people also experience problems in swallowing or language disturbances. These auras typically occur in order, usually with visual first, then sensory, then motor or language disturbances. This what we term a migraine ‘march’.
Migraine Physiology: Cortical Spreading Depression (CSD)
Past and current research generally agrees that the key principle behind a migraine is what is known as a ‘cortical spreading depression’ (CSD). This process is not completely understood due to the complexity of our brain physiology and the difficulty in obtaining direct experimental data, but we do understand the basics. A typical healthy human brain has roughly 100 billion neurons. Clearly, as many of us know, neurons are specialised cells in our brain that transmit and receive signals using chemical and electrical pathways. As soon as the neuron receives a signal from another neuron it transmits an electrical charge sending the message down an axon (a branch like structure that protrudes from the neuron cell body) which then eventually reaches a tiny gap called a synapse. Here the signal is transmitted via a neurotransmitter across the gap which binds onto a receptor site at the other side of the synapse. On the other side of the synapse is a dendrite of yet another nearby neuron which propagates the message again.
The Role of cell membranes in CSD
One neuron may have up to 7000 synaptic connections with other neurons. The electrochemical energy that neurons use for signalling pathways is generated by an exchange of ions (potassium and sodium) across their cell membranes. These ions exist in different concentrations either side of a cell membrane. This exchange occurs because there are tiny sodium-potassium pumps that exist in the membrane of each cell allowing ions to pass in and out. These little pumps allow three sodium ions to leave the cell and two potassium ions to enter. Hence there is a net export of a single positive charge per pump cycle. This inequality of ion transfer produces a charge, maintaining a polarized membrane with the inner surface slightly negative in relation to the outer surface. This flux across the cell membrane causes an exchange in electrochemical energy or what we call the cell membrane potential. This is quite important when it comes to neurons generating signals necessary for communicating with other neurons.
How CSD affects Ion Exchange
Our brains utilise about 20% of our total energy requirement. However, the activation of these tiny little pumps alone in our cell membranes use about half of the total energy that the brain receives! Cortical Spreading Depression (CSD) is a process that interrupts and disturbs the ion concentration inside and outside a neuron. Locally in a cell, CSD is characterised by a massive redistribution of ions across the neuron membranes. The neurons ultimately lose their membrane potential leading to depolarisation and a depression in any normal electrochemical activity. This leads to in effect a silencing of brain activity. The silencing sweeps across our brains like a wave causing disturbances in our vision and other sensory changes we described earlier. The aura of migraine lasts from 5 to 60 minutes, and usually happens before the headache. Migraine without aura clearly does not include this stage. Unfortunately, CSD appears to also stimulate the next phase in migraine which is called the trigeminovascular system. The leads to the headache.
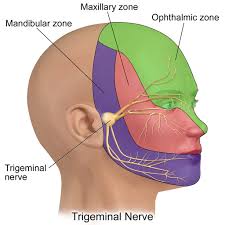
The headache is typically throbbing and made worse by movement. Some people describe a pressing or tightening pain. It is usually on one side of the head, especially at the start of an attack. However, it is not uncommon to get pain on both sides, or all over the head. Nausea and vomiting can happen at this stage, and you may feel sensitive to light or sound, or both. Research of migraine suggests that the physiology of this phase is intimately linked to the trigeminal nerve.
Migraine Physiology: The Trigeminal Nerve
The trigeminal nerve is one the 12 cranial nerves that send and receive signals to and from our body. The trigeminal is also the largest cranial nerve and its main function is transmitting sensory information to the skin, sinuses, and mucous membranes in the face. It also stimulates movement in the jaw muscles. The trigeminal nerve centre (or ganglion) allied with these other functions also consists of other neurons that innervate important blood vessels in our brain.
What appears to happen is that CSD activates the trigeminal nerve resulting in inflammation and vasodilation of blood vessels in the brain. During a migraine the trigeminal ganglion releases powerful chemicals and proteins that cause blood vessels to dilate. Hence the term trigeminovascular system. In fact, one of the most common medication for migraines are triptans, which work by narrowing the blood vessels in the brain. Triptans can unfortunately cause side effects like dizziness and drowsiness and have to be used with caution for people with heart conditions. In November this year there has been some encouraging news for migraines sufferers as there is a new medication that is pending approval. Ubrogepant is pending approval by the US Food and Drug Administration and manufacturer Allergan says they have plans to get licensed in Europe and Asia as well. Ubrogepant, is an oral pill that instead works by blocking a protein called GCRP (calcitonin gene-related peptide) in the nervous system, which is involved in pain signalling, blunting any discomfort.
Migraine Medications: Triptans
In a trial conducted by the Montefiore Headache Centre in New York, Ubrogepant was given to a sample group of 1,686 migraine sufferers in differing doses: some were given 25mg, others 50mg and the rest, a placebo pill. In those who were given 25mg, 20 per cent felt pain free after two hours and 34 per cent said they no longer felt sensitive to light or noise or felt sick – the most common side effects of a migraine. In the higher dose group, 22 per cent felt totally pain free within 120 minutes and nearly 40 per cent had been alleviated of other symptoms as well. Although these findings mean Ubrogepant is not as effective as many triptans (which cause 40 per cent to be pain free and 75 per cent to have no side effects) they are useful because they get around the problems for those with heart conditions.
A migraine usually lasts from four to 72 hours. How often migraines occur varies. After an attack, you might feel drained, confused and washed out for up to a day. Some people report feeling elated. Sudden head movement might bring on the pain again briefly. Interestingly we do treat quite a few people for migraines at the clinic and this is not widely known within the general public. We work by helping to relieve the effects of stress in the head, neck and shoulders. Whilst there are many different triggers for migraines this is always one that is worth exploring.